How to treat scarring and skin damages resulted from acne is of great concern to patients with moderate to severe acne. Failed or inadequate treatment of acne is a major cause in development of acne scars and early intervention is critical. The same distress acne patients experience may follow with its disfiguring sequels. Psychological burden of acne scars is perceived to be grievous for stigmatized way these patients are viewed in our society.
The incidence of acne related scars is not known. It is frequently stated that scars are consequence of severe inflammatory nodulocystic acne lesions occurring deep in the dermis. Although it may exist with only minor more superficial/mild acne.
It is very likely that some patients are further prone to scarring based on the factors that define their skins. Of paramount importance that acne should be treated early and adequately. Despite advances in various therapeutic approaches, multitude of these treatments are unsatisfactory to patients and leads to their frustrations and disappointments due to either several associated adverse effects or inadequate resolution.
Following factors are stated as involved in etiology and introduced as precipitants for scar formation following acne.
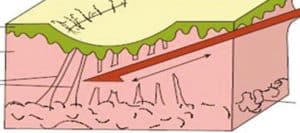
The following wound healing scenario explains the pathology and alterations in deeper layers of skin, connective tissue and skin pigmentation following acne. Acne as well as any other cause for a minor wound may follow the same pathway. The inflammatory phase at the pilosebaceous gland is more severe and prolonged in patients with post-acne scarring comparing to those with no post-acne sequel [1].
The initial step is defined by a structured series involving inflammatory cells. This succession of episodes is arranged by neutrophils. Subsequently, macrophages, fibroblasts and platelets elaborate a variety of cytokines, which create an environment prone to granulation tissue constitution [2].
Eventually, migration of fibroblasts coincide with proliferation and recapitulation by depositing new collagen. Simultaneously, production of new capillaries is triggered by some factors released in the wound section. Among them, platelet-derived growth factor, firbolbast growth factor and trnsforming frowth facotrs alpha and beta, which further stimiulate migaration and proliferation of fibroblasts [3].
This proliferatory phase of fibroblasts and collagen depostion initiates within four days and predominates by collagen type III replacing by collagen type I as wound matures over time [4].
Matrix remodelling phase continues with fibroblasts and kertinocytes generation of enzymes such as matrix metaloproteinases (MMPs), which are degrading enzymes responsible for a lytic function within extrcellular matrix [5]. A problem arises when this organized cascade is disrupted by its anabolic and catabolic phases. The balance between metaloproteinases and their inhibitors determines formation of either hypertorphic scars or atrophic lesions [6].
An overreacting wound healing response may happen, creating a bulgy lesion of fibrotic tissue, hypertophic scar. Alternatively, deleted connective tissue is deficiently replaced and forms a pitted appearance resembling the surface of a golf ball, atrophic scar. In either case, the scar often is a legacy of skewed healing process. Pathology of spots and discolorations resulted from acne, however, have less correlation with anabolic and catabolic stages, rather, skin pigmentation changes arise prominently.
Types are the most important factor in determining its appropriate treatment. There are basically two types of scars. One is associated with propagated tissue generation and the other is associated with some tissue loss
Keloids: They present as smooth, firm, irregularly shaped lesions. Upper body or angle of the jaw are more prone to these type of facial scarring. Skin of dark-complexions (black skin) is more predisposed to develop hypertrophic scars. They could be regarded as thick, raised, lobulated fibrotic plaques. Types with increased skin tissue rarely observed with acne even in prolonged severe cases.
Acne spots: Flat discolorations either brown or red.They are more likely to fade away either gradually without treatment or using fading creams. Post inflammatory pigmentations are classified in the same category. Blocks of pink hyperpigmentations seen following skin breakouts and more likely prolonged acne.
Ice-pick lesions, rolling scars, box car scars: they all associated with some degree of depression in the skin but the shape of the scar within the skin is different. For icepick scars the depression is in the form of a triangle with an opening 4mm. They may be superficial or deep, fairly linear but irregular and generally turn out on the cheeks. These lesions are variably resistant to the treatments and the more penetrating they are the longer it takes to be healed totally. Acne lesions can lead to ice pick scars.

Acne scars in form of icepick and boxcar scarring
Depressed fibrotic scars: They present as large with sharp margins and steep sides. Their base is rigid, white and can not be stretched. They may result from severe lesions such as cystic and nodular forms of acne. Read more on depressed scars and their management.

Acne scars of rolling type
This type of lesions manifest as soft, distensible, ivory-white in color and small in size (few millimeter in diameter). Acne is recurrently associated with atrophic scars. Acne scarring is outcome of improper deposition of collagen and elastin and insufficient wound repair process.
Lining epithelium is not flat and atrophic but hyperplastic. Healing them involves inducement of the skin’s repair mechanisms and rebuilding elastin and other fibers. Overall they have a good prognosis. They do not expand in size or number over time. However, aging has an adverse effect on acne caused scarring and render them more pronounced.
| Grade | Level of Disease | Example of Scars |
|---|---|---|
| 1 | Macular | Erythematous, hyper or hypo pigmented flat marks, a problem of color rather than contour, visible to the patient or observer at any distance |
| 2 | Mild | Mild rolling, small soft papular, may not be obvious at social distance > 50cm; may be covered by makeup or shadow of shaved beard hair in men |
| 3 | Moderate | More significant rolling, shallow boxcar, mild to moderate hypertrophic or papular scars; obvious at social distances of 50cm; not easily covered; able to be flatened by manual stretching of the skin (if atrophic) |
| 4 | Severe | Punched out atrophic (deep boxcar), ice pick, bridges and tunnels, marked atrophy dystrophic significant hypertrophy or keloid; obvious at social distances, not easily covered, and not able to be flattened by manual stetching of the skin |
The more acne inflammation persists the more likely development of acne scar is. Treatment promptly in its course is the best method for prevention of acne damages. Use of anti oxidants as a preventive method especially vitamin E is still viewed with skepticism, some studies even report a harmful effect. Powerful anti oxidants such as lipoic acid when employed alone works with no success. A favorable medication for acne essentially address the following problems:
An elevated sebaceous glands production, overproduction of epithelial cells lining follicles, bacterial involvement, acne inflammation. Read also next page for more prevention tips. Another treatment that has been used by Mayo is application of butulinum toxin to help more effective of natural repair system by reducing muscle tension around the wound.
It seems that muscle spasm has a detrimental effect on regeneration of collagen fibers even if we could for a moment ignore a decrease in blood circulation and inflammatory response secondary to muscle spasm.
Most have heard of chemical peels, dermabrasion, silicone injections, collagen implants and laser treatment since these have been widely publicized in the lay press for treating scars. For the patient whose acne has recently cleared, it is worthy to know that scars tends to become less apparent with time and that any consideration of cosmetic surgery must be deferred for some time.
Mild post inflammatory pigmentations tend to disappear in a few months. More severe cases of post inflammatory pigmentations in may benefit from azelaic acid and hydroquinone [7]. It ought to be pointed out that scarring lesions on the body does not tend to improve as readily and is conventionally less amenable to cosmetic surgery. One study suggests an average reduction of 31% after 3 sessions of percutaneous collagen induction [8].
Subcision surgery technique for treatment of acne scarring
Retinoic acid, alpha and beta hydroxy peels, such as glycolic acid, potent anti oxidants such as alpha lipoic acid creams are widely discussed and debated in acne scar treatment of lesions including acne hyperpigmentation spots, scars and lack of skin uniformity.
Among medications, retinoic acid preparations are more well-known and well-studied. Despite showing some degree of improvement, its use alone does not bring about a dramatic conversion in acne scarring. Skin dryness and redness are among complications. Atrophic acne scar may be satisfactorily treatment in many patients, but multiple methods are often required to ensure the best outcomes [9].
acne scar excision (subcision): This surgical method of treatment uses a scalpel or punch to remove the damaged skin. Under local anesthesia, the lesion is excised and the skin edges are then sutured together. Excision is typically recommended to patients with deep pitted marks that are not amendable to the TCA technique. Good for deeper marks. Longer recovery time.
Iontophoresis:
New study suggests use of tretinoin for improvement of acne caused scars with either tretinoin or estriol. In iontophoresis an ionizable drug is injected into the skin using an electrical discharge without use of a needle.
Dermabrasion involves controlled surgical scraping that resurfaces the outermost layers of the skin to give a smoother appearance. It can be done over the full surface of the face or on small areas. Dermabrasion also may be done in conjunction with other cosmetic procedures such as a chemical peeling or face lift. Dermabrasion is used to treat a range of skin imperfections including:
Wrinkles and frown lines, pre-cancerous skin growths (keratoses), face scarring (excluding burn scars, acne scars), post-surgery marks, skin pigmentation, sun damage, tattoos, age spots, facial freckles, acne discoloration spots and other forms.

Acne scars combination therapy with dermabarsion followed by chemical peels
Acupuncture
Use of acupuncture for scar repair is considered a new approach. Use of small, very thin needles in the skin precipitates a tiny injury at its site which is associated with an increase in skin microcirculation and stimulation of inflammatory mediators.
Infiltration of cytokines is chemotactic for fibroblasts and production of new collagen. Acupuncture seems to be rather effective in improving appearance of atrophic scars. Facial cosmetics acupuncture is becoming more popular not only for treatment of acne-related ailments but for other rejuvenating purposes.
Another technique for acne scar removal appear to be more with a desirable outcome in convex regions of the face. Lateral cheek and the temples do not benefit from this office procedure as much. Laser treatment could be associated with hyperpigmentation (increased skin color) or hypopigmentation (decreased skin color) for short or long term in treatment vicinity. Scars, infection and persistent redness are also possible side effects of laser resurfacing. With available medications these could be controlled.
Some clinical testing suggest that high-energy, pulsed CO2 laser can safely and effectively improve or even eliminate atrophic acne scars and provides many contributions in contrast with traditional treatment means. The use of nonablative laser systems is a good treatment alternative for patients with atrophic scarring who are unable or unwilling to endure the prolongs postoperative recovery process associated with ablative laser skin resurfacing procedures [10].
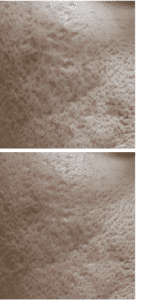
Acne scarring treated with adipose tissue stem cells, top)before bottom)after stem cell therapy
Erbium, the latest technique, has generated more satisfactory results which leads to elimination of a superficial scarring and a reduction in other forms of scars [11]. One study suggests laser resurfacing with more effective result using laser punch-out method.
Some research indicate that old severe scarring responds substantially less to laser acne scars treatment while newly formed marks could almost completely vanish. This indicates that timing of treatment could be significant. Laser also have been utilized to treat acne particularly in patients who show sensitivity reactions to medications for acne. Interestingly, outcomes are not very promising, skin irritation and cost is among other considerations.

Depth of infiltration of various laser types into the skin with scarring
Skin resurfacing at-home regimen to treat acne scars and to reconstruct the skin by helping to rebuild collagen:
High potency serums have been bioengineered for collagen remodeling within dermis layer, stimulation of skin’s natural healing mechanisms and skin resurfacing. Enriched with many anti aging elements, the serum for getting rid of acne scars alters skin tone and texture dramatically while enforce dermal repair.
Reactivation of growth factors such as epidermal growth factor, by Tripeptide-5 has been addressed by international journal of cosmetic science. This new molecule may help more uniform alignment of collagen and other connective tissue’s fibers, which in turn help reorganization of collagen fibers that has been disrupted during scar formation. One of these growth factors affected by Tripeptide-5 is TGF-beta, transforming growth factor, which play a significant role in tissue regeneration, dermal repair and cell proliferation.
Refacing treatment serum minimizes and tightens the pores, smooth away cutaneous damages.
Retexturizing treatment speeds the cell renewal of epidermis zone and assist with rapid evacuation of dead cells.
Kojic acid, a natural ingredient, notably more friendly to the skin compare to its rival, hydroquinone. In harmony with nature, Kojic acid has been found to eliminate hyperpigmentation spots, freckles, discolorations resulted from acne and refine the skin by revealing a brighter, more even-toned complexion
Acne scar treatment which enhances the epidermal circulation and as a result helps to activate the natural collagen synthesis of dermal layer of the skin may be rendered robust in elimination of acne scar.
Bioflavanoids, green tea extract and alpha lipoic acid are among other vehicles to target skin scarring which can act through activation of natural dermal/epidermal function to rebuild itself. Any skin care product which takes advantage of these potent antioxidants to subside skin oxidation of lipids as this mechanism implicated in skin ability to repair itself. This protective effect delays collagen deterioration and premature aging.
Facial aging is another constituent, which deteriorates scarred skin. With aging, the facial skin starts to sag and seems to literally hang on the scars. The inelastic strands of scars bind the skin, giving it an uneven, more wrinkled appearance. This is amplified by other age-correlated transitions such as atrophy of facial skeletal muscles and loss of collagen and skin’s connective tissue. The four-piece formula has been bioengineered to address all these insidious progressive changes.
Skin resurfacing serum for acne scar comes with three other formulations, day effect cream, facial exfoliator and dermal repair serum. The cream maintains work of the night serum during the day and while it is very healing to the skin, it has its own skin resurfacing properties and is intended for skin repair. To better understand how Dermal Repair serum works please follow the links on your right. See also our frequently asked questions for more info.
References:
1. Holland DB, Jeremy AHT, Roberts SG, Seukeran DC, Layton AM, Cunliffe, WJ.
. Brit J Dermatol. 2004;150(1):72-81.
2. Martin P, Leibovich SJ. Inflammatory cells during wound repair, the good, the bad and the ugly. Trends in Cell Biology. 2005;15(11):599-607.
3. Stadelmann WK, Diggenis AG, Tobin GR. Physiology and healing dynamic of chronic cutaneous wounds. Am J Surg. 1998;176(2A):26S-38S.
4. Baum CL, Arpey CJ. Normal cutaneous wound healing: clinical correlation with cellular and molecular events. Derm Surg. 2005;31(6):674-86.
5. Midwood KS, Williams LV. Schwarzbauer JE. Tissue repair nd the dynamics of the extracellular matrix. Int J Biochem Cell Biol. 2004;36(6):1031-7.
6. Chivot M. Pawin H, Beylot C, et al. Scars epidemiology, physiopathology, clinical features and treatment. Ann de Dermatol et de Venerol. 2006;133(10):813-24.
7. Fabbrocini G, De Vita V, Monfrecola A, De Padova MP, Brazzini B, Teixeira F, Chu A. Percutaneous collagen induction: an effective and safe treatment for post-acne scarring in different skin phototypes. J Dermatolog Treat. 2012;not yet in print.
8. Levy LL, Zeichner JA. Management of acne scars II, a comparative review of non-laser-based, minimally invasive approaches. Am J Clin Dermatol. 2012;13(5):331-40.
9. Goodman GJ. Postacne scarring: a review of its pathophysiology and treatment. Dermatol Surg. 2000;26(9):857-71.
10. Tanzi EL, Alster TS. Comparison of a 1450-nm diode laser and a 1320-nm Nd: YAG laser in the treatment of atrophic facial scars: a prospective clinical and histologic study. Dermatol Surg;2004(2 pt1):152-7.
11. Yoon JH, Park EJ, Kwon IH, et al. Concomitant use of an infrared fractioanal laser with low-dose isotretinoin for the treatment of acne and acne scar.
12. Soddard MA, Hermann J, Moy L, Moy R. Improvement of atrophic acne scars in skin of color using topical synthetic epidermal growth factors, EGF serum. JDD; 2017(volume16-issue4).
13. Drono B, Tan J, Layton AM et al. How people with facial acne scarring are perceived in society, an online survey. Dermatol Ther 2016Jun (6)2: 207-218.
14. Alam S, Dover JS. Treatment of acne scarring. Skin Therapy Letter 2005, volume11;number10.